

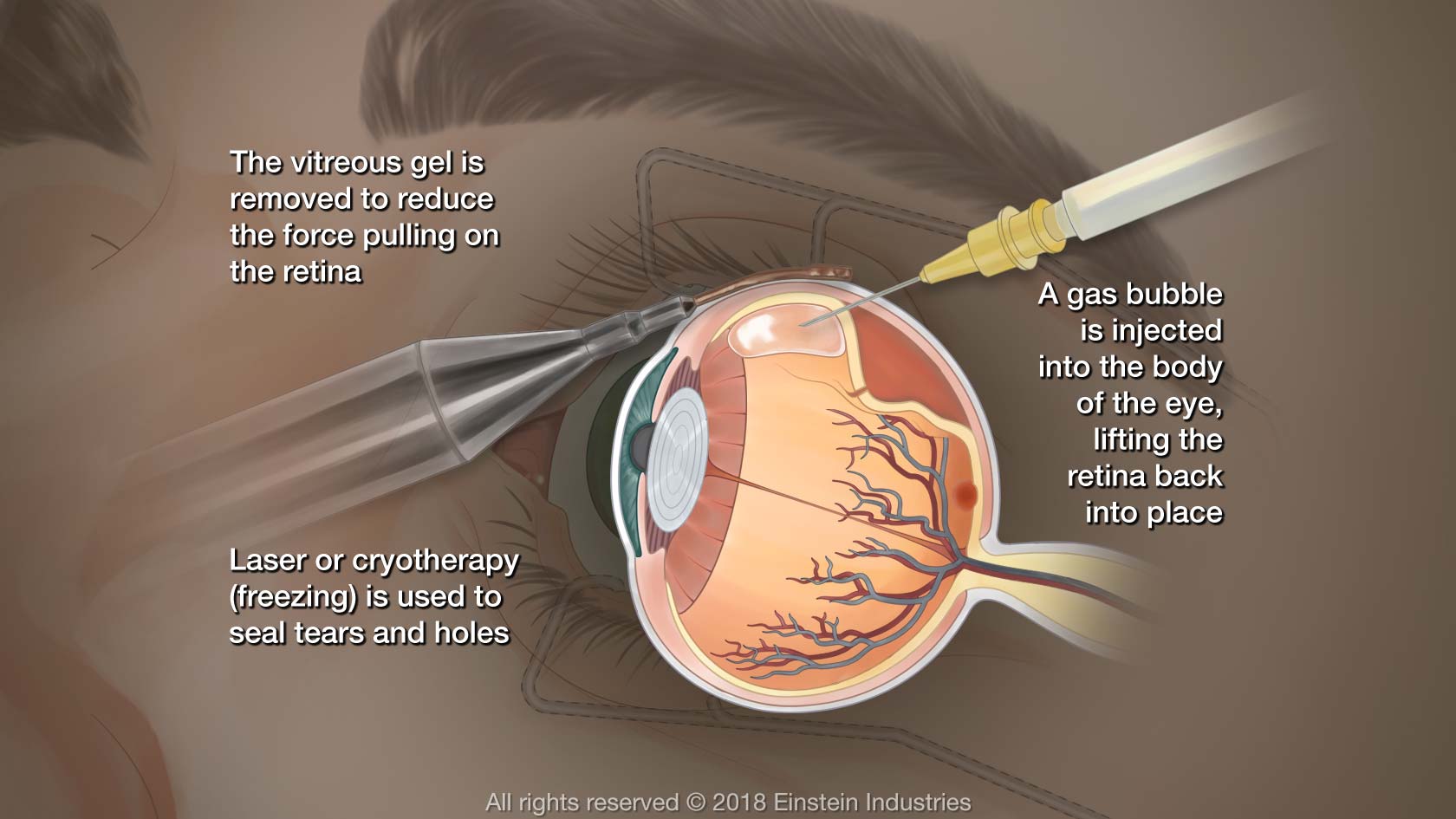
This method of repair allows the neurosensory retina to slowly reattach to the pigment epithelial layer, resulting in a high-integrity retinal attachment.

The buoyancy and surface tension of the gas bubble closes the retinal tear and allows the pigment epithelial layer to absorb the subretinal fluid. RRDs that involve the superior retina-i.e., between the 8 and 4 o’clock positions-have one to two breaks no farther apart than one clock hour and have no evidence of fixed retinal folds, holes with rolled edges or vitreous hemorrhage are especially suitable for PnR surgery. Approximately 40 percent of patients who present with RRD can be managed with PnR surgery. The procedure usually takes between 15 and 20 minutes. It’s performed using topical anesthesia in the office or in an outpatient setting. PnR is the least invasive surgery and is especially suitable for phakic patients. 6 Since PnR and SB surgery don’t result in cataract formation, they should be considered as the first options in the repair of RRD.ġ. It also demonstrated that the age of patients with detachments ranged from 55 to 59 years.
#RETINA DETACHMENT SURGERY SUCCESS RATE FULL#
The Netherlands study of 2,998 cases revealed that a full two-thirds, or 66.5 percent, of patients who presented with retinal detachments were phakic. It’s important for the vitreoretinal surgeon to realize that the majority of patients who present with retinal detachments are phakic. Lens Status and Age of Patients Who Present With RRD In this article, I’ll outline the indications and techniques of PnR, SB and PPV surgery and discuss the complications of PPV surgery in phakic patients. I feel strongly that teaching PnR and SB surgery should be an integral part of any vitreoretinal fellowship training program. 1,2 These programs teach only PPV surgery in the management of RRD and accept the complication of cataract formation within one to two years and its sequelae. Many fellowship training programs in the United States, Europe and Australia no longer teach PnR and SB surgery, despite the fact that studies have shown that the anatomic and visual results of these procedures are better than PPV surgery, especially in young, phakic patients. The development of small-gauge vitrectomy units with high-speed cutters, wide-angle viewing systems, the use of intraocular gases SF6 and C3F8 and perfluorocarbon liquid has revolutionized the repair of RRD and led to the misconception that PnR and SB surgery are no longer necessary in the management of RRD. We start by teaching the indications and benefits of the least invasive procedures, i.e., PnR and SB, and proceed with the indications and benefits of the more invasive PPV surgery.
#RETINA DETACHMENT SURGERY SUCCESS RATE SERIAL#
In our fellowship training program, we teach a serial approach to the repair of RRD. By teaching all three methods in our vitreoretinal fellowship, we ensure that our graduate surgeons will be well equipped to address the many varieties of detachments with the appropriate procedure and achieve the best anatomic and visual results. I’ve been involved in the training of 60 vitreoretinal fellows, including 29 from the United States, 11 from Canada and 12 from Australia. In this article, I’ll review the current methods of rhegmatogenous retinal detachment repair, which include pneumatic retinopexy, scleral buckling and pars plana vitrectomy, and I’ll discuss the University of British Columbia approach to detachment surgery. I n any surgery, the goal should be to perform the least invasive procedure to repair the pathology and to avoid intraoperative and postoperative complications.


 0 kommentar(er)
0 kommentar(er)
